Ok, everyone knows how to give a thumbs up, but do you REALLY know how to give a thumbs up? To do this we need to focus on the Abductor Pollicus Longus, a muscle of the forearm. This muscle gives us some insight into common thumb and wrist injuries.
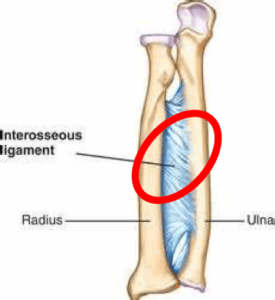
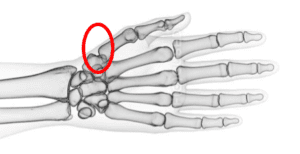
The Abductor Pollicis Longus originates from the body of the ulna, interosseous ligament, and the middle third portion of the radius. The muscle belly ends into a long tendon, which inserts into the radial side base of the first metacarpal bone. This is a bone at the base of the thumb. The nerve that innovates this muscle is the posterior interosseous nerve, a deep branch of the radial nerve.
Why is this muscle important?
It’s because it abducts and extends the thumb. That is, it allows you to thumbs up!
However, this muscle is implicated in a few common thumb and wrist injuries, such as de Quervain’s tenosynovitis, whereby the tendons of the Abductor Pollicus Longus and the Extensor Pollicus Brevis may become irritated and gliding becomes impaired. Symptoms are often characterised by pain, tenderness and swelling of the thumb side of the wrist.
De Quervain’s tenosynovitis is often classified as a repetitive strain injury (RSI), however there are complex interactions between genetic factors and biopsychosocial factors that can contribute to the painful symptoms (Peters‐Veluthamaningal, van der Windt, Winters, & Meyboom‐de Jong, 2009).
Treatment of de Quervain’s tenosynovitis may be operative or non-operative, with the majority of patients improving with conservative treatment involving physiotherapy (stretching and strengthening), splinting and corticosteroid injections (Ilyas, 2009; Ippolito, Hauser, Patel, Vosbikian, & Ahmed, 2018).
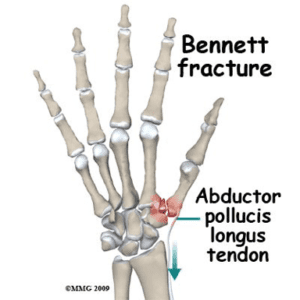
The Abductor Pollicus Longus can be affected by traumatic injuries such as the Bennett fracture, usually sustained by a fall on an extended thumb, or upon hard impact of a closed fist (Brownlie & Anderson, 2011). This is predominately due to where the Abductor Pollicus Longus attach in the hand (base of first metacarpal bone).
Due to the complexity of the injury, Bennett fractures are usually treated under the management of specialist hand surgeons.
– Stacy Koh, Physiotherapist
If you would like to make an appointment with one of our physiotherapists, give one of our friendly team members a call on 4724 0768 or click here to book online!
References:
Brownlie, C., & Anderson, D. (2011). Bennett fracture dislocation Review and management. Australian Family Physician, 40, 394-396.
Ilyas, A. M. (2009). Nonsurgical Treatment for de Quervain’s Tenosynovitis. Journal of Hand Surgery, 34(5), 928-929. doi:10.1016/j.jhsa.2008.12.030
Ippolito, J. A., Hauser, S., Patel, J., Vosbikian, M., & Ahmed, I. (2018). Nonsurgical Treatment of De Quervain Tenosynovitis: A Prospective Randomized Trial. Hand (New York, N.Y.), 1558944718791187-1558944718791187. doi:10.1177/1558944718791187
Peters‐Veluthamaningal, C., van der Windt, D., Winters, J. C., & Meyboom‐de Jong, B. (2009). Corticosteroid injection for de Quervain’s tenosynovitis. Cochrane Database of Systematic Reviews(3). doi:10.1002/14651858.CD005616.pub2


